Missy's Hope Equine Rescue Resource
General Information:
Mission and Policy Information
Our Programs:
The Chey/Annie Project Fundraisers
The Chey/Annie Project Accounting
The Chey/Annie Project Future Sling Locations
Rescue Information:
Resources:
Pet Food and Product Warnings and Recalls
Congressional Information:
Letter Writing Campaigns For Horses
Horse Health Information:
Cushings/Insulin Resistance Information
Helping Your Horse Prepare For Being Blind
Articles Relating To Equine Blindness
Miscellaneous:
Cushings/Insulin Resistance Information
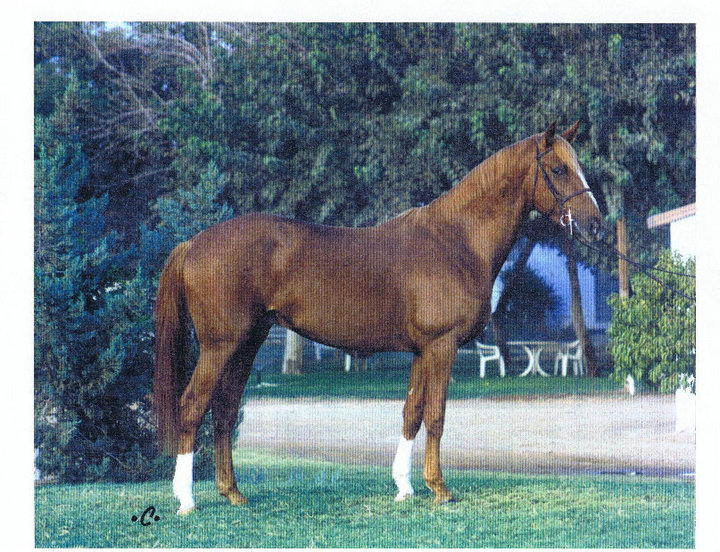
Meet Fleet. Fleet is the reason I have added this page to my site. He came into our family after the loss of Missy. He lived in a stable in Michigan where he was a lesson horse prior to joining our family. A worker from his stable saw my ad looking for a horse to be a companion to Missy's mom, CC, and told me about how he was facing euthanasia because he could no longer jump. The stable owner assured me that there was nothing else wrong with him. Fleet was only 18 at the time. This is Fleet as he looked the day he arrived at our farm, 21 October 2006. We were not told about his Cushing's prior to his arrival.
Here is Fleet in March of 2007. You can see the weight loss that has occurred over the winter (all my other pictures show him in blankets, this was the first warm day we had). Although it is hard to see from this picture Fleet had four inch long hair all over. In May 2007 we discovered that Fleet was having trouble shedding his winter hair coat in addition to the weight loss that he was still suffering with. At this point, we had increased his feed to triple what he started with. His teeth had been floated in October before he arrived and we were told they typically had them done once a year unless needed more. In June 2007, we finally had a diagnosis of Cushings for Fleet. It took a lot of wonderful people helping us to pinpoint what was wrong. It turned out that once we mentioned the trouble losing his winter coat that a member of a rescue group that I was in contact with suggested it. Without that suggestion, we would have never even known what Cushings was. I didn't take any pictures this month, but Fleet had lost almost 200 lbs from the time he arrived in October. The weight loss began to be noticeable in December and continued until the middle part of July. It slowed down in July after the medication and the emergency diet for Cushings horses were started. Fleet's previous owners will still not admit that they knew of his Cushings before he came to us. Looking at all the records that they sent with him, his feeding routine was almost exactly the diet used for Cushings horses along with many of the supplements used. The only thing missing is mention of Pergolide or Chasteberry, both of which are sometimes used for horses with Cushings (Note: Pergolide and Chasteberry cannot be used at the same time.). Here is Fleet in August 2007. He was just starting to respond to the medication and diet for Cushings. You can see the dramatic weight loss that he faced from the Cushings. You can also see the beginning of his muscle wasting.
This is Fleet from the left side. You can see his ribs and how little barrel he has from all the weight loss.
This is Fleet from the rear taken Aug 2007. Note the protrusion of his hip bones.
Here is a picture of Fleet taken in October 2007. You can see that he has gained some weight back in his barrel area. The ribs are still noticeable, but the groove between them is not as deep. Fleet was also recovering from an illness in this picture. I hope to get more pictures if we can get a warm day. He gets too cold already this winter, so he wears a lightweight blanket during the day and a warmer one at night.
This Fleet from the rear in October 2007. His hip bones are showing still and the muscle wasting is more evident. He has not gained any fat on his top line yet. the good news is that the muscle wasting has slowed and he is starting to show some improvement in his chest and rump as time goes on. I will continue to update the pictures of Fleet as we battle the Cushings. It is my hope that we can continue to increase his weight and his muscle mass with time and work. I only wish that I had been told that he had Cushings. It would not have mattered to me in the slightest, but it would have saved him suffering and he would still be that sleek shiny horse that he was when he arrived here. Fleet is a wonderful horse that loves our children and is so easy to be around. He brightens every day with his nickers. We will do all that we can for him until the time comes that he is ready to cross the rainbow bridge. We hope that the time for that will not come before he is at least in his 40's or later. Here are pictures I took on a warmer day in January 2008
This is Fleet from the front. Fleet from the back (wondering what the heck I am doing standing behind him!)
Fleet left side and Fleet right side (somewhat). He was very happy with me when I gave him his blanket back after the photo session! These pictures were just taken August 2008.
Fleet is still struggling somewhat with his Cushings. He lost weight again as spring came on, but is starting to gain it back again. These pictures don't show how much weight he has gained in his chest area! He has also started gaining just a bit along his topline. I mentioned how concerned I was to the vet and he said that he thought Fleet was doing very well. He couldn't believe how much Fleet changes each time he comes to visit. He also said that at Fleet's age, he may not get the topline back up the way it used to be. Fleet is very much the dominate horse in his little group of him and CC. He doesn't show it unless it is time to eat though. For his age (which we learned is actually between 23 and 25 based on his teeth presentation (not the 20 he would be which was what the original owners claimed!), he is a happy and spunky horse. He still doesn't break a trot very often, but the other day when the heat and humidity had gone down quite a bit, I saw him out cantering across the pasture!
Fleet update 29 Oct 2009. Fleet sure has come a long way! We have switched him over to Safe Choice feed (he gets 4 pounds a day split between 2 meals) and free choice Alfalfa. I am so grateful that our feed stores finally started carrying this wonderful product! It has made an enormous difference for Fleet!
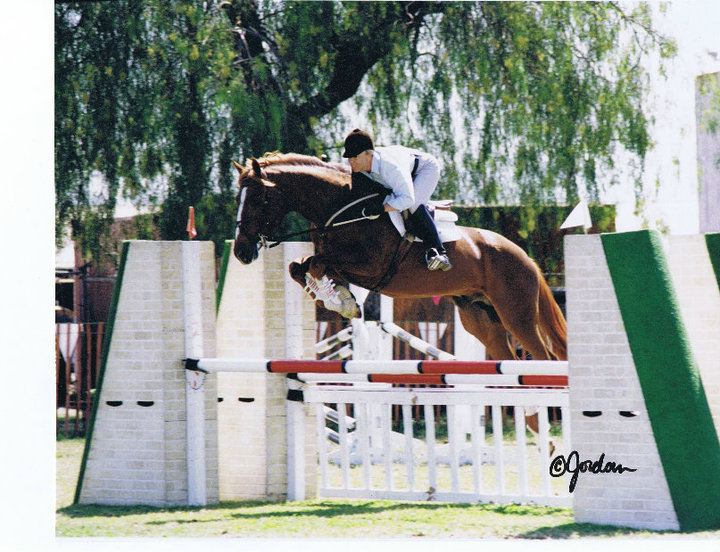
Amazing isn't it? He did have an issue with abscesses just before these pictures were taken (he found a way to sneak his buddy's feed and it cost him big time!). I think it is just the time of year and the massive amounts of rain and snow we have had this past month. I don't have boots for him, so he is wearing a diaper full of medicine, covered by a plastic baggie, which is then covered with duct tape (the duct tape helps keep his feet from cutting through the diaper and plastic so quickly!). His abscesses are almost healed at this point and he is feeling much better. We recently were able to locate Fleet's original breeder. This boy has had an amazing life! The best news is that he is really 21 years old and his real name is Teddy. He answers to Teddy much better than he ever answered to Fleet...now if I can just remember to call him that! Here are some pictures of him that his breeder sent from when he was younger.
Isn't he stunning? I sure think so.
Here are some pictures that we took in August 2010. This was right after we moved into our new house. They are a little farther away than I would like. When it warms up (it is 4 Jan 2011 and a brisk 15 degrees out!), I will take some updated pictures of him for on here.
|
||||||||||||||
|
|